Page 19 - SAM September 2019
P. 19
PUBLIC HEALTH
form the necessary consultations and diag-
nostics on a same-day to next-day basis.
Transportation
Patients that face the combined
dilemma of clinical amputation risk and
socioeconomic barriers frequently cite
transportation as a primary barrier to care.
However, many private insurance plans
and Medicare Advantage plans offer trans-
portation as a benefit. Medicaid will soon
provide transportation for all beneficiaries
through all managed and traditional carri-
ers. A little energy from office staff can go
a long way to help patients acquire the
“free” transportation included in their
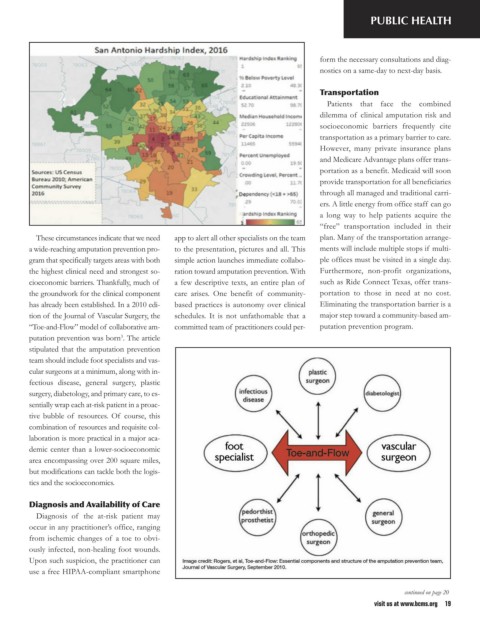
These circumstances indicate that we need app to alert all other specialists on the team plan. Many of the transportation arrange-
a wide-reaching amputation prevention pro- to the presentation, pictures and all. This ments will include multiple stops if multi-
gram that specifically targets areas with both simple action launches immediate collabo- ple offices must be visited in a single day.
the highest clinical need and strongest so- ration toward amputation prevention. With Furthermore, non-profit organizations,
cioeconomic barriers. Thankfully, much of a few descriptive texts, an entire plan of such as Ride Connect Texas, offer trans-
the groundwork for the clinical component care arises. One benefit of community- portation to those in need at no cost.
has already been established. In a 2010 edi- based practices is autonomy over clinical Eliminating the transportation barrier is a
tion of the Journal of Vascular Surgery, the schedules. It is not unfathomable that a major step toward a community-based am-
“Toe-and-Flow” model of collaborative am- committed team of practitioners could per- putation prevention program.
putation prevention was born . The article
3
stipulated that the amputation prevention
team should include foot specialists and vas-
cular surgeons at a minimum, along with in-
fectious disease, general surgery, plastic
surgery, diabetology, and primary care, to es-
sentially wrap each at-risk patient in a proac-
tive bubble of resources. Of course, this
combination of resources and requisite col-
laboration is more practical in a major aca-
demic center than a lower-socioeconomic
area encompassing over 200 square miles,
but modifications can tackle both the logis-
tics and the socioeconomics.
Diagnosis and Availability of Care
Diagnosis of the at-risk patient may
occur in any practitioner’s office, ranging
from ischemic changes of a toe to obvi-
ously infected, non-healing foot wounds.
Upon such suspicion, the practitioner can
use a free HIPAA-compliant smartphone
continued on page 20
visit us at www.bcms.org 19