Page 18 - Layout 1
P. 18
OPIOID CRISIS
OMAPNIAOGIIDNGTLHONEGR-TAEPRYM
IN TODAY’S RISK-CONSCIOUS CLIMATE
By Maxim S. Eckmann, MD and Ameet Nagpal, MD, MS, MEd
PAIN: A SYMPTOM AND A DISEASE all physicians and non-physician providers, including those in pri-
A portion of the population that experiences se- mary care, inpatient care and surgery — just to name a few — should
adapt to the current climate and seek understanding of harm reduc-
vere acute pain or injury will go on to experience per- tion and risk management when dealing with patients with difficult
sistent pain long after apparent healing of damaged pain problems.
tissues, for months or even years (1). This pain serves
no useful function in terms of recovery, and it is ex- LONG TERM OPIOID THERAPY FOR
ceedingly frustrating and distressing for patients, pa- PERSISTENT PAIN
tients’ families, and health care professionals.
Persistent pain and subsequent costs have quietly be- Opioids, being relatively flexible, tolerable, potent and familiar op-
come an epidemic in the industrialized world. In the tions for physicians, have long been a mainstay of treating moderate
United States, direct and indirect costs likely exceed to severe acute pain. In the 1990s, pain societies advocated for more
$500 billion annually, placing major stress on the U.S.
health care system (2). The growth in the chronic
pain patient population has been followed by an epi-
demic of prescription opioid addiction and overdose
deaths due to the high exposure rate of patients to
opioids while under medical care.
The field of pain medicine has evolved in recent
years to try and understand the pain “continuum” as
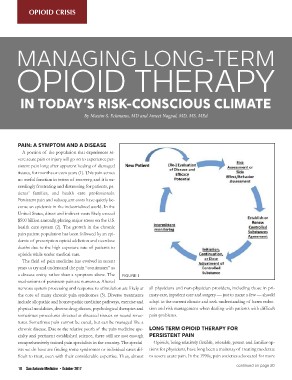
a disease entity rather than a symptom alone. The FIGURE 1
mechanisms of persistent pain are numerous. Altered
nervous system processing and response to stimulation are likely at
the core of many chronic pain syndromes (3). Diverse treatments
include allopathic and homeopathic medicine pathways, exercise and
physical modalities, diverse drug classes, psychological therapies and
sometimes procedures directed at diseased tissues or neural struc-
tures. Sometimes pain cannot be cured, but can be managed like a
chronic disease. Due to the relative youth of the pain medicine spe-
cialty and pertinent established science, there still are not enough
comprehensively trained pain specialists in the country. The special-
ists we do have are finding some syndromes or individual cases dif-
ficult to treat, even with their considerable expertise. Thus, almost
18 San Antonio Medicine • October 2017 continued on page 20